Melanosis Neurocutaneous is a rare condition that affects both the skin and the nervous system. Ever wondered what makes this disorder so unique? Melanosis Neurocutaneous involves the presence of large or multiple pigmented moles on the skin, often accompanied by neurological issues. These can range from seizures to developmental delays. The condition is usually present at birth or develops in early childhood. Understanding Melanosis Neurocutaneous can help in early diagnosis and management, improving the quality of life for those affected. Ready to dive into 30 intriguing facts about this rare condition? Let’s get started!
Key Takeaways:
- Melanosis Neurocutaneous is a rare disorder causing pigmented skin lesions and neurological issues. Early diagnosis and multidisciplinary care can improve prognosis and quality of life for affected individuals.
- Ongoing research and support groups offer hope for better understanding and management of Melanosis Neurocutaneous. Awareness and early intervention can make a significant difference in the lives of those affected.
What is Melanosis Neurocutaneous?
Melanosis Neurocutaneous is a rare congenital disorder characterized by the presence of large or multiple pigmented skin lesions and neurological abnormalities. This condition can affect various parts of the body, including the brain and spinal cord. Here are some intriguing facts about this unique condition.
-
Melanosis Neurocutaneous is also known as Neurocutaneous Melanosis (NCM).
-
The disorder is often associated with large congenital melanocytic nevi (CMN), which are pigmented skin lesions present at birth.
-
NCM is a non-hereditary condition, meaning it is not passed down from parents to children.
-
The exact cause of NCM is unknown, but it is believed to result from abnormal development of melanocytes during embryonic growth.
Symptoms and Diagnosis
Understanding the symptoms and how Melanosis Neurocutaneous is diagnosed can help in early detection and management.
-
Symptoms can vary widely but often include seizures, developmental delays, and hydrocephalus (accumulation of fluid in the brain).
-
Neurological symptoms usually appear within the first two years of life.
-
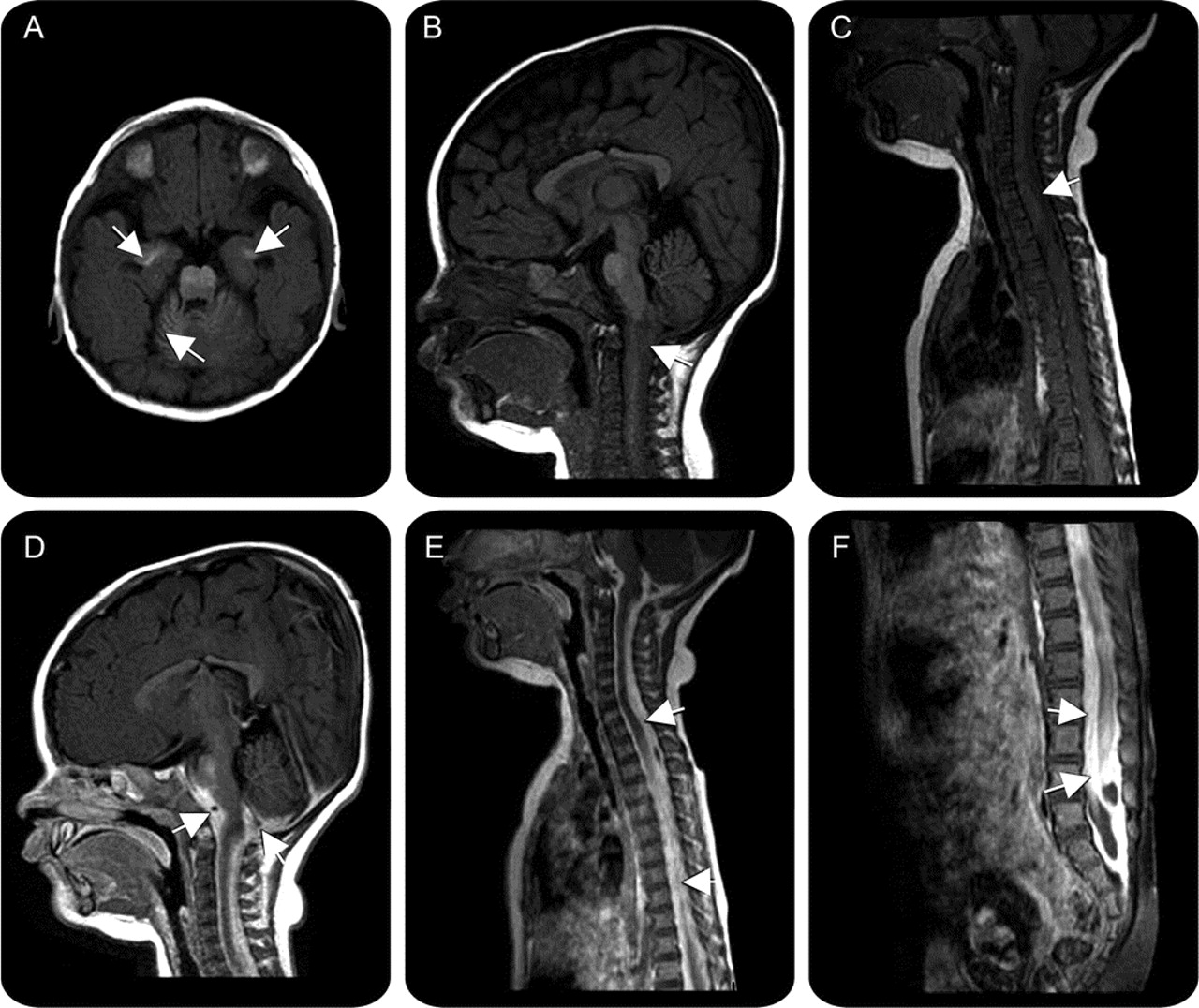
Diagnosis typically involves a combination of physical examination, imaging studies like MRI, and sometimes a biopsy of the skin lesions.
-
MRI scans can reveal melanotic deposits in the brain and spinal cord, which are indicative of NCM.
Treatment Options
While there is no cure for Melanosis Neurocutaneous, various treatments can help manage symptoms and improve quality of life.
-
Treatment often focuses on managing neurological symptoms, such as using anticonvulsant medications for seizures.
-
Surgical interventions may be necessary to remove large or problematic skin lesions.
-
Hydrocephalus may require the placement of a shunt to drain excess fluid from the brain.
-
Regular monitoring and follow-up with a multidisciplinary team are crucial for managing the condition effectively.
Prognosis and Life Expectancy
The prognosis for individuals with Melanosis Neurocutaneous can vary based on the severity of symptoms and the presence of complications.
-
Life expectancy can be reduced, especially if severe neurological complications arise.
-
Early intervention and management of symptoms can improve the overall prognosis.
-
Some individuals with mild symptoms may lead relatively normal lives with appropriate medical care.
Research and Future Directions
Ongoing research aims to better understand Melanosis Neurocutaneous and develop more effective treatments.
-
Genetic studies are being conducted to identify potential genetic markers associated with NCM.
-
Researchers are exploring the role of stem cell therapy in treating neurological symptoms of NCM.
-
Advances in imaging technology are helping to improve the accuracy of diagnosis and monitoring.
-
Clinical trials are underway to test new medications that may help manage symptoms more effectively.
Support and Resources
Support from healthcare professionals and patient organizations can make a significant difference for individuals with Melanosis Neurocutaneous and their families.
-
Patient support groups provide a platform for sharing experiences and information.
-
Specialized clinics and hospitals offer comprehensive care for individuals with NCM.
-
Online resources and forums can connect patients and families with others facing similar challenges.
-
Educational materials and workshops can help families better understand and manage the condition.
Interesting Historical Facts
The history of Melanosis Neurocutaneous offers some fascinating insights into how our understanding of the condition has evolved over time.
-
The first documented case of NCM was reported in the early 19th century.
-
Early medical literature often confused NCM with other neurocutaneous disorders.
-
Advances in medical imaging in the late 20th century significantly improved the diagnosis and understanding of NCM.
-
Historical case studies have contributed to the development of current treatment protocols.
Famous Cases and Awareness
Highlighting notable cases and raising awareness can help bring attention to this rare condition.
-
Some well-documented cases of NCM have been featured in medical journals and conferences.
-
Awareness campaigns and advocacy groups work to educate the public and healthcare professionals about NCM.
-
Increased awareness can lead to earlier diagnosis and better outcomes for individuals with Melanosis Neurocutaneous.
Final Thoughts on Melanosis Neurocutaneous
Melanosis neurocutaneous, though rare, presents a unique set of challenges and insights into the human body. Understanding its symptoms, causes, and treatments can help those affected manage their condition better. Knowledge about this disorder not only aids patients but also informs medical professionals and researchers.
By spreading awareness, we can foster a supportive community for those living with melanosis neurocutaneous. Remember, early diagnosis and intervention are key to managing any medical condition effectively. Stay informed, consult healthcare providers regularly, and support ongoing research to improve treatment options.
Informed individuals can make a significant difference in the lives of those affected by this condition. Keep learning, stay curious, and share your knowledge to help others navigate their health journeys.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
