Oculo-Gastrointestinal Muscular Dystrophy (OGMD) might sound like a mouthful, but understanding it can be straightforward. This rare genetic disorder affects muscles in the eyes and digestive system, leading to a range of symptoms. OGMD often starts with droopy eyelids and difficulty swallowing, progressing to more severe muscle weakness. It's caused by mutations in specific genes responsible for muscle function. While there's no cure yet, treatments focus on managing symptoms and improving quality of life. Knowing the facts about OGMD can help those affected and their families navigate this challenging condition. Let's dive into 25 key facts about Oculo-Gastrointestinal Muscular Dystrophy.
Key Takeaways:
- Oculo-Gastrointestinal Muscular Dystrophy (OGMD) affects eye and digestive muscles, causing symptoms like drooping eyelids and difficulty swallowing. Early diagnosis and management are crucial for a better quality of life.
- Understanding OGMD's genetic basis and symptoms can lead to better diagnosis and management. Support groups, assistive devices, and regular check-ups help those with OGMD live well.
What is Oculo-Gastrointestinal Muscular Dystrophy?
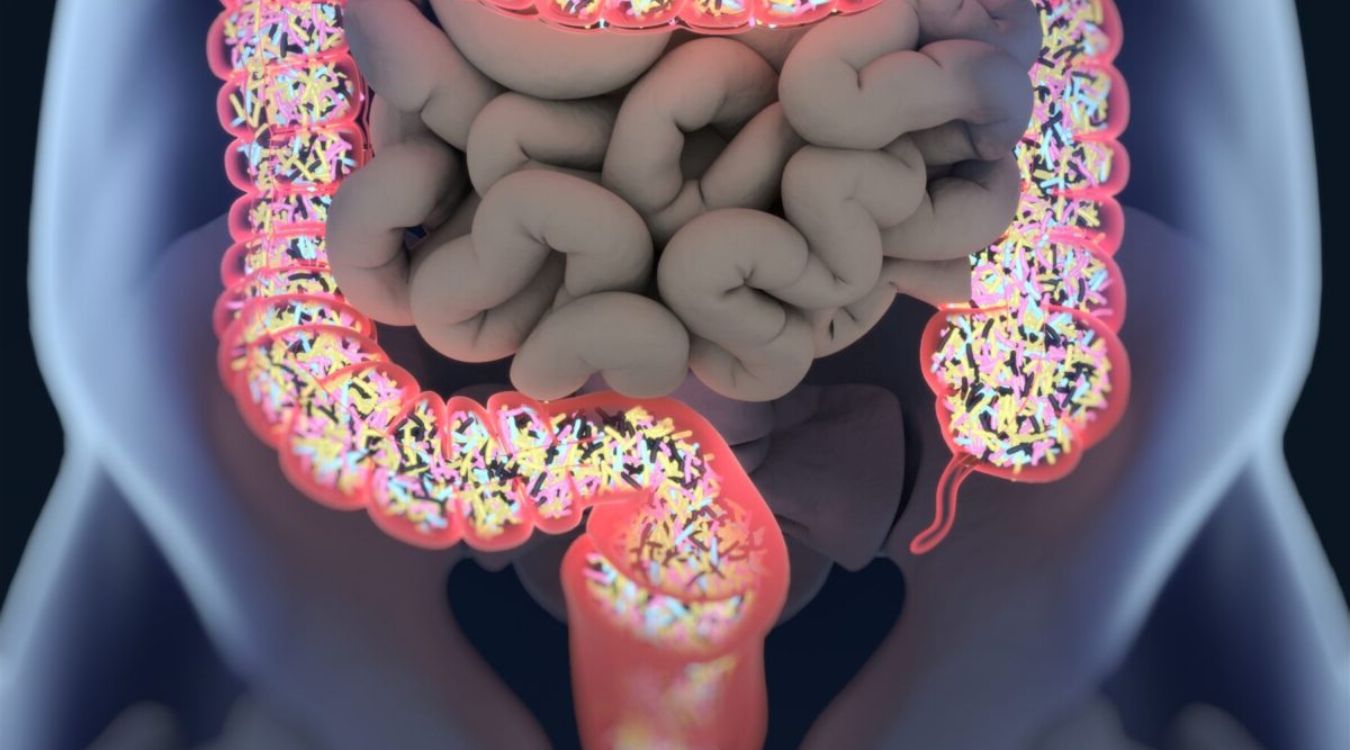
Oculo-Gastrointestinal Muscular Dystrophy (OGMD) is a rare genetic disorder affecting muscles around the eyes and digestive system. Understanding this condition can help those affected and their families manage symptoms better.
-
OGMD primarily affects muscles around the eyes and digestive system. This means patients often experience difficulty with eye movements and digestive issues.
-
It is a genetic disorder. OGMD is inherited, meaning it is passed down from parents to children through genes.
-
Symptoms usually appear in childhood. Most individuals start showing signs of OGMD in their early years, though the severity can vary.
-
It is a progressive disease. Symptoms worsen over time, making early diagnosis and management crucial.
Symptoms of OGMD
Recognizing the symptoms of OGMD can lead to earlier diagnosis and better management of the condition.
-
Drooping eyelids (ptosis) are common. Many patients experience difficulty keeping their eyes open due to weak muscles.
-
Difficulty swallowing (dysphagia) often occurs. Weak muscles in the digestive system can make swallowing food challenging.
-
Frequent eye movement problems. Patients might struggle with moving their eyes in different directions.
-
Digestive issues like constipation. Weak muscles in the digestive tract can lead to chronic constipation.
Causes and Genetics of OGMD
Understanding the genetic basis of OGMD can provide insight into its development and potential treatments.
-
OGMD is caused by mutations in specific genes. These genetic mutations disrupt normal muscle function.
-
It follows an autosomal recessive inheritance pattern. Both parents must carry the mutated gene for a child to develop OGMD.
-
Genetic testing can confirm a diagnosis. Identifying the specific gene mutation helps in diagnosing OGMD accurately.
-
Family history plays a significant role. A history of OGMD in the family increases the likelihood of inheriting the condition.
Diagnosis and Testing
Accurate diagnosis is essential for managing OGMD effectively. Various tests and evaluations help in confirming the condition.
-
Muscle biopsy is often used. Examining a small sample of muscle tissue can reveal characteristic changes of OGMD.
-
Electromyography (EMG) tests muscle activity. EMG helps assess the electrical activity of muscles, indicating weakness.
-
Genetic testing identifies specific mutations. This test confirms the presence of gene mutations responsible for OGMD.
-
Clinical evaluation by a neurologist. A specialist can assess symptoms and recommend appropriate tests.
Treatment and Management
While there is no cure for OGMD, various treatments can help manage symptoms and improve quality of life.
-
Physical therapy strengthens muscles. Regular exercises can help maintain muscle function and delay progression.
-
Speech therapy aids in swallowing. Techniques taught by a speech therapist can make swallowing easier.
-
Nutritional support is crucial. A dietitian can recommend foods that are easier to swallow and digest.
-
Surgical options for severe ptosis. Surgery can help lift drooping eyelids, improving vision.
Living with OGMD
Living with OGMD requires adapting to challenges and finding ways to maintain a good quality of life.
-
Support groups provide emotional help. Connecting with others facing similar challenges can be comforting.
-
Assistive devices can improve mobility. Tools like walkers or wheelchairs help maintain independence.
-
Regular medical check-ups are essential. Monitoring the condition helps manage symptoms effectively.
-
Education about the condition is vital. Understanding OGMD empowers patients and families to make informed decisions.
-
Advocacy for research and awareness. Supporting research can lead to better treatments and increased awareness of OGMD.
Final Thoughts on Oculo-Gastrointestinal Muscular Dystrophy
Oculo-Gastrointestinal Muscular Dystrophy (OGMD) is a rare condition that affects both the eyes and digestive system. Understanding OGMD can help those affected and their families manage symptoms more effectively. Early diagnosis is crucial for better treatment outcomes. Genetic testing and regular check-ups are essential for monitoring the progression of the disease.
Support from healthcare professionals, family, and patient communities can make a significant difference in the quality of life for those with OGMD. Staying informed about the latest research and treatment options is also vital.
By spreading awareness and sharing knowledge, we can contribute to a better understanding of this rare condition. Remember, every bit of information helps in the fight against OGMD. Stay curious, stay informed, and support those who are navigating this challenging journey.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
