Lymphomatoid papulosis (LyP) might sound intimidating, but understanding it can make a world of difference. This rare skin disorder, often mistaken for other conditions, presents as recurring, self-healing bumps or lesions. Despite its alarming appearance, LyP is typically benign. However, it shares characteristics with lymphomas, making awareness crucial. LyP affects people of all ages, though it’s more common in adults. Symptoms can vary widely, leading to misdiagnosis. Knowing the facts about LyP helps in recognizing and managing it effectively. From its causes and symptoms to treatment options, we’ll cover everything you need to know about this perplexing condition.
Key Takeaways:
- Lymphomatoid Papulosis (LyP) is a rare skin disorder that looks like a rash but is actually a type of cancer called lymphoma. It can be itchy and painful, but lesions often heal on their own, leaving scars.
- While there is no cure for LyP, treatments like topical steroids and light therapy can help manage symptoms. Regular monitoring and joining support groups can provide emotional and practical support for those living with LyP.
What is Lymphomatoid Papulosis?
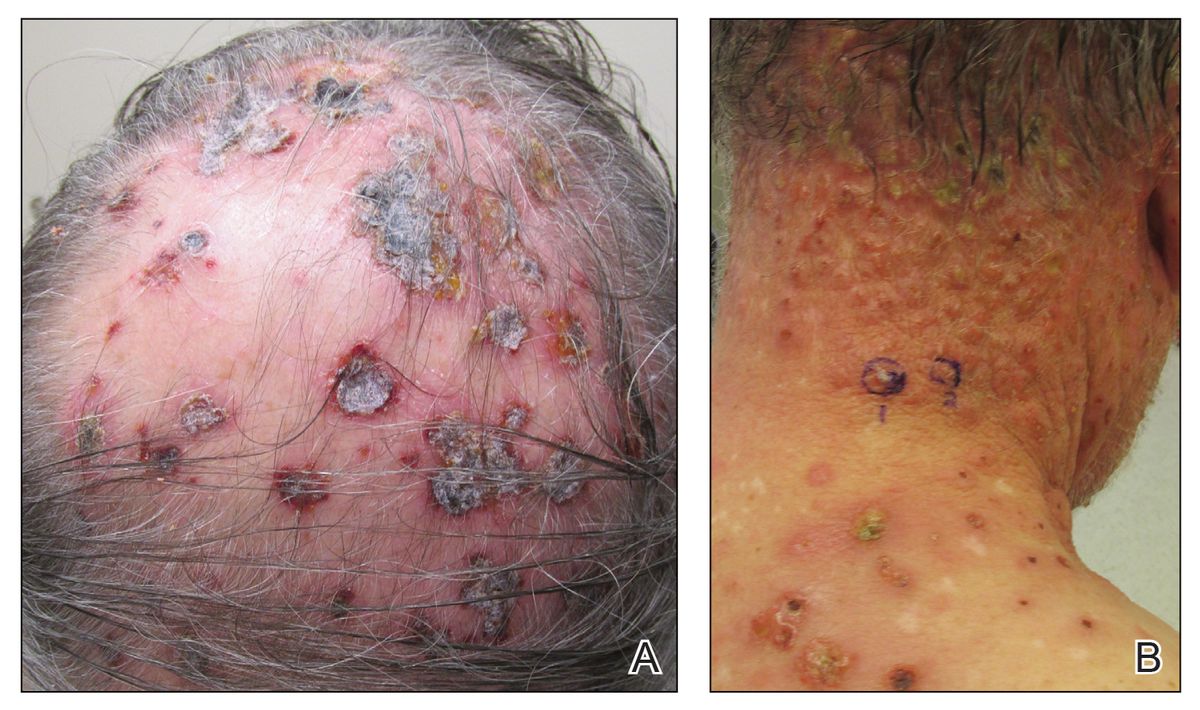
Lymphomatoid papulosis (LyP) is a rare skin disorder that can be quite confusing due to its appearance and behavior. It looks like a rash but is actually a type of lymphoma. Here are some fascinating facts about LyP that will help you understand this condition better.
-
Rare Condition: LyP affects only about 1 to 2 people per million each year. This makes it a very rare disorder.
-
Chronic Disease: LyP is a chronic condition, meaning it can last for many years, often with periods of remission and flare-ups.
-
Benign but Malignant: Although LyP lesions appear benign, they are actually a form of lymphoma, which is a type of cancer.
-
Age Range: LyP can affect individuals of any age, but it is most commonly diagnosed in adults between 30 and 50 years old.
-
Gender Prevalence: Both men and women can develop LyP, but it is slightly more common in men.
Symptoms and Diagnosis
Understanding the symptoms and how LyP is diagnosed can help in managing the condition effectively.
-
Skin Lesions: The primary symptom of LyP is the appearance of skin lesions that can look like pimples or small bumps.
-
Itching and Pain: These lesions can be itchy or painful, adding to the discomfort.
-
Self-Healing Lesions: One of the unique features of LyP is that the lesions often heal on their own, leaving behind scars.
-
Biopsy for Diagnosis: A skin biopsy is usually required to diagnose LyP, as the lesions can resemble other skin conditions.
-
Misdiagnosis: Due to its rarity and similarity to other skin disorders, LyP is often misdiagnosed initially.
Causes and Risk Factors
The exact cause of LyP remains unknown, but several factors may contribute to its development.
-
Genetic Factors: There may be a genetic component, as some cases of LyP have been reported in families.
-
Immune System: An abnormal immune response is believed to play a role in the development of LyP.
-
No Known Triggers: Unlike some other skin conditions, there are no known environmental or lifestyle triggers for LyP.
-
Associated Conditions: LyP can be associated with other types of lymphomas, such as Hodgkin's lymphoma or mycosis fungoides.
-
Risk of Progression: Although rare, there is a small risk that LyP can progress to a more aggressive form of lymphoma.
Treatment Options
While there is no cure for LyP, various treatments can help manage the symptoms and reduce the frequency of flare-ups.
-
Topical Steroids: These can help reduce inflammation and itching associated with LyP lesions.
-
Phototherapy: Light therapy, or phototherapy, is another treatment option that can help clear up lesions.
-
Systemic Medications: In more severe cases, systemic medications like methotrexate may be prescribed.
-
Regular Monitoring: Regular follow-ups with a dermatologist are crucial to monitor the condition and adjust treatment as needed.
-
Lifestyle Adjustments: While there are no specific lifestyle changes that can prevent LyP, maintaining overall skin health can be beneficial.
Living with LyP
Living with LyP can be challenging, but understanding the condition can make it easier to manage.
-
Emotional Impact: The chronic nature of LyP can take an emotional toll, leading to stress or anxiety.
-
Support Groups: Joining support groups can provide emotional support and practical advice from others who have LyP.
-
Education: Educating yourself and others about LyP can help reduce misunderstandings and stigma associated with the condition.
-
Skin Care Routine: Establishing a gentle skin care routine can help manage symptoms and prevent irritation.
-
Stay Informed: Keeping up with the latest research and treatment options can empower you to make informed decisions about your care.
Final Thoughts on LyP Facts
LyP, or lymphomatoid papulosis, might sound intimidating, but understanding it helps. This rare skin disorder, marked by recurring lesions, often gets mistaken for more severe conditions. Despite its alarming appearance, LyP usually has a good prognosis. Treatments range from topical steroids to light therapy, depending on severity. Regular check-ups are crucial since LyP can sometimes be linked to lymphomas. Awareness and early diagnosis make managing LyP easier. If you or someone you know shows symptoms, consult a dermatologist. Knowledge empowers, and staying informed about LyP ensures better health outcomes. Keep these facts in mind, and don't let the medical jargon scare you. Stay proactive, stay informed, and take control of your health journey.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
