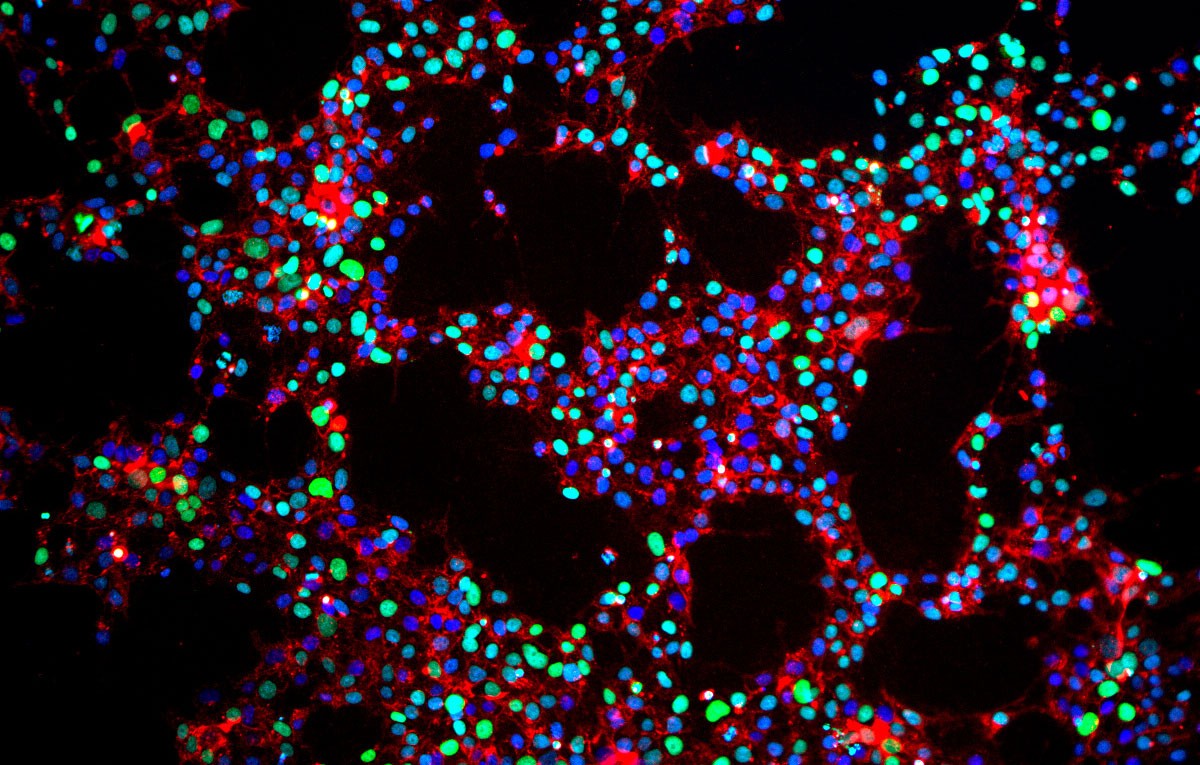
Induced pluripotent stem cells (iPSCs) are a groundbreaking discovery in the field of regenerative medicine. These cells are created by reprogramming adult cells to an embryonic-like state, allowing them to develop into any cell type in the body. iPSCs hold immense potential for treating diseases, studying development, and testing new drugs. Unlike embryonic stem cells, they don't involve the ethical concerns of using embryos. Scientists can generate iPSCs from a patient's own cells, reducing the risk of immune rejection. This innovation opens doors to personalized medicine, offering hope for conditions like Parkinson's, diabetes, and heart disease. Dive into these 36 fascinating facts to understand the magic behind induced pluripotent stem cells.
What Are Induced Pluripotent Stem Cells?
Induced pluripotent stem cells (iPSCs) are a groundbreaking discovery in the field of regenerative medicine. They are adult cells reprogrammed to an embryonic-like state, capable of differentiating into various cell types. Here are some fascinating facts about iPSCs.
-
iPSCs were first created in 2006 by Shinya Yamanaka and Kazutoshi Takahashi. They used four specific genes to reprogram adult mouse fibroblasts into pluripotent stem cells.
-
The four genes used for reprogramming are Oct4, Sox2, Klf4, and c-Myc. These genes are often referred to as "Yamanaka factors."
-
iPSCs can differentiate into any cell type in the body. This makes them incredibly valuable for research and potential therapies.
-
They are derived from adult cells, such as skin or blood cells. This avoids the ethical issues associated with embryonic stem cells.
-
iPSCs have the same genetic makeup as the donor. This reduces the risk of immune rejection in potential therapies.
How Are iPSCs Created?
Creating iPSCs involves a complex process of reprogramming adult cells. This section delves into the steps and techniques used to generate these versatile cells.
-
Reprogramming involves introducing specific genes into adult cells. This is typically done using viral vectors.
-
Non-viral methods, such as plasmid transfection, are also being explored. These methods aim to reduce the risk of insertional mutagenesis.
-
The reprogramming process can take several weeks. Cells must be carefully monitored to ensure successful conversion.
-
iPSCs are typically cultured in a special medium. This medium supports their growth and maintains their pluripotency.
-
The efficiency of reprogramming is relatively low. Only a small percentage of cells successfully become iPSCs.
Applications of iPSCs
iPSCs have a wide range of applications in medicine and research. They offer new possibilities for disease modeling, drug discovery, and regenerative therapies.
-
iPSCs can be used to model diseases in the lab. Researchers can study disease mechanisms and test potential treatments.
-
They are valuable for drug discovery and testing. iPSCs can be differentiated into specific cell types to screen for drug efficacy and toxicity.
-
iPSCs hold promise for regenerative medicine. They could potentially be used to replace damaged tissues or organs.
-
They are being explored for use in personalized medicine. iPSCs derived from a patient's own cells could be used to create personalized treatments.
-
iPSCs can be used to study early human development. Researchers can gain insights into developmental processes and congenital disorders.
Challenges and Limitations
Despite their potential, iPSCs face several challenges and limitations. Understanding these obstacles is crucial for advancing their use in medicine.
-
Reprogramming efficiency is low. Improving this efficiency is a key area of research.
-
There is a risk of genetic mutations during reprogramming. These mutations could potentially lead to cancer.
-
iPSCs can form teratomas when injected into animals. This highlights the need for careful control of their differentiation.
-
The use of viral vectors poses safety concerns. Non-viral methods are being developed to address this issue.
-
Differentiating iPSCs into specific cell types is challenging. Researchers are working to develop more reliable differentiation protocols.
Ethical Considerations
iPSCs offer a more ethically acceptable alternative to embryonic stem cells. However, they still raise some ethical questions.
-
iPSCs avoid the ethical issues associated with embryonic stem cells. They do not require the destruction of embryos.
-
There are concerns about the use of genetic modification. The long-term effects of reprogramming are not fully understood.
-
The potential for cloning raises ethical questions. iPSCs could theoretically be used to create cloned organisms.
-
Informed consent is crucial when obtaining donor cells. Donors must be fully aware of how their cells will be used.
-
There are concerns about the commercialization of iPSC technology. Ensuring equitable access to therapies is important.
Future Directions
The future of iPSCs is bright, with ongoing research aimed at overcoming current challenges and expanding their applications.
-
Researchers are working to improve reprogramming efficiency. New methods and factors are being explored.
-
Efforts are underway to develop safer reprogramming techniques. Non-viral methods and small molecules are being investigated.
-
Advances in gene editing could enhance iPSC technology. Techniques like CRISPR could be used to correct genetic defects.
-
iPSCs could play a role in organ transplantation. Bioengineered organs created from iPSCs could address the organ shortage.
-
Personalized medicine is a major focus. iPSCs could be used to create patient-specific treatments.
Interesting Facts About iPSCs
Beyond their scientific and medical significance, iPSCs have some intriguing aspects that highlight their versatility and potential.
-
iPSCs have been used to create mini-brains in the lab. These organoids can be used to study brain development and diseases.
-
They have been used to create beating heart cells. This has potential applications in cardiac research and therapy.
-
iPSCs can be used to study rare diseases. Patient-specific iPSCs can model diseases that are difficult to study otherwise.
-
They have been used to create insulin-producing cells. This could lead to new treatments for diabetes.
-
iPSCs have been used to generate blood cells. This has potential applications in treating blood disorders.
-
They can be used to study the effects of aging. iPSCs can be derived from older individuals to study age-related diseases.
The Power of Induced Pluripotent Stem Cells
Induced pluripotent stem cells (iPSCs) have revolutionized science and medicine. These cells, reprogrammed from adult cells, can become any cell type in the body. This ability opens doors for regenerative medicine, disease modeling, and drug discovery. Researchers can study diseases in a dish, leading to better treatments and understanding. iPSCs also reduce the need for embryonic stem cells, addressing ethical concerns.
Their potential in personalized medicine is immense. Doctors could use a patient’s own cells to treat conditions, minimizing rejection risks. While challenges remain, like ensuring safety and efficiency, the progress is promising. The journey of iPSCs from discovery to application showcases human ingenuity and the relentless pursuit of knowledge. As research continues, the impact of iPSCs on healthcare and science will only grow, offering hope and solutions for many medical challenges.
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
