Wilson-Mikity Syndrome is a rare lung condition affecting newborns, primarily premature infants. Named after pediatricians Dr. Robert Wilson and Dr. Victor Mikity, who first described it in 1960, this syndrome is characterized by rapid, unexplained respiratory distress. Symptoms often include rapid breathing, grunting, and cyanosis (bluish skin due to lack of oxygen). Unlike other lung diseases in newborns, Wilson-Mikity Syndrome doesn’t always show immediate signs at birth but can develop within the first few weeks of life. Diagnosis typically involves chest X-rays and clinical observation. While the exact cause remains unknown, researchers believe it may be linked to lung development issues in the womb. Treatment focuses on supportive care, such as oxygen therapy and mechanical ventilation if needed. Early detection and intervention can significantly improve outcomes for affected infants.
Key Takeaways:
- Wilson-Mikity Syndrome mainly affects premature babies, causing rapid breathing and low oxygen levels. Early recognition and proper treatment are crucial for managing this rare lung condition.
- Research is ongoing to improve understanding and treatment of Wilson-Mikity Syndrome. Scientists are focusing on genetic studies, better diagnostic tools, and preventive measures to enhance long-term outcomes for affected infants.
What is Wilson-Mikity Syndrome?
Wilson-Mikity Syndrome (WMS) is a rare lung condition primarily affecting premature infants. It was first described in 1960 by pediatricians Robert Wilson and Victor Mikity. The syndrome is characterized by rapid breathing and poor oxygenation, often leading to chronic lung disease. Here are some intriguing facts about this rare condition:
-
Premature Infants: WMS mainly affects babies born before 32 weeks of gestation. Their lungs are not fully developed, making them more susceptible.
-
First Described in 1960: Pediatricians Robert Wilson and Victor Mikity first identified the syndrome. Their research laid the groundwork for understanding this rare condition.
-
Rapid Breathing: Infants with WMS often exhibit tachypnea, which means they breathe faster than normal. This is due to their underdeveloped lungs struggling to get enough oxygen.
-
Poor Oxygenation: These infants frequently have low blood oxygen levels. This can lead to cyanosis, where the skin turns a bluish color due to lack of oxygen.
-
Chronic Lung Disease: Many infants with WMS develop chronic lung disease, requiring long-term medical care and monitoring.
Symptoms and Diagnosis
Recognizing the symptoms early can make a significant difference in managing WMS. Here are some key symptoms and diagnostic methods:
-
Grunting Sounds: Infants may make grunting noises while breathing. This is a sign that they are working hard to breathe.
-
Retractions: The skin between the ribs may pull in with each breath. This indicates difficulty in breathing.
-
Nasal Flaring: Widening of the nostrils during breathing is another symptom. It shows the infant is trying to take in more air.
-
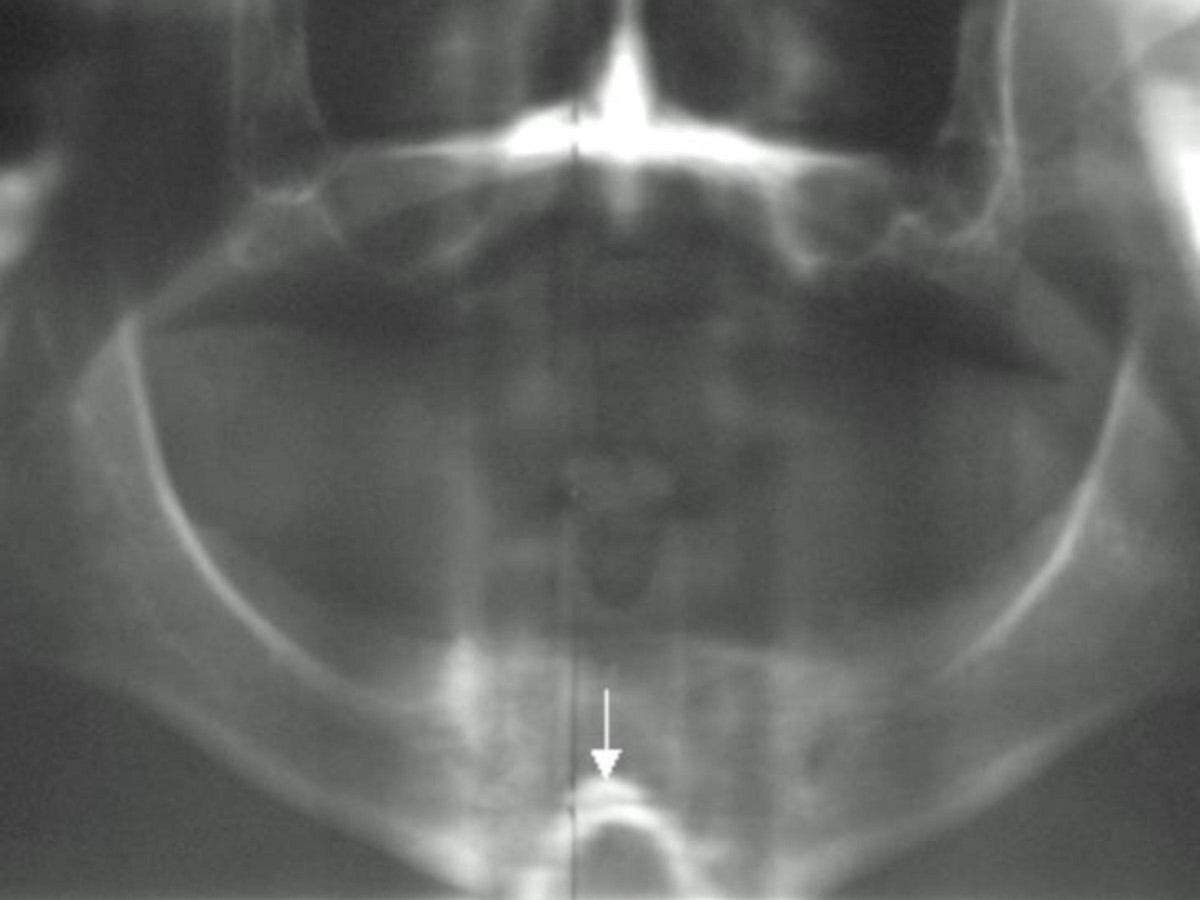
Chest X-rays: Doctors use chest X-rays to diagnose WMS. The images can show characteristic patterns in the lungs.
-
Blood Gas Analysis: This test measures oxygen and carbon dioxide levels in the blood. It helps assess how well the lungs are functioning.
Causes and Risk Factors
Understanding what causes WMS and the risk factors involved can help in prevention and early intervention:
-
Prematurity: The primary cause is being born prematurely. The earlier a baby is born, the higher the risk.
-
Low Birth Weight: Babies with low birth weight are more susceptible to WMS. Their underdeveloped organs struggle to function properly.
-
Lung Development Issues: Incomplete lung development is a significant risk factor. The lungs may not have enough surfactant, a substance that helps keep them open.
-
Genetic Factors: Some studies suggest a genetic predisposition. Families with a history of lung diseases may have a higher risk.
-
Infections: Prenatal infections can increase the risk. Infections can interfere with lung development.
Treatment and Management
Managing WMS involves a combination of medical interventions and supportive care. Here are some common treatments:
-
Oxygen Therapy: Many infants require supplemental oxygen. This helps maintain adequate oxygen levels in the blood.
-
Mechanical Ventilation: In severe cases, mechanical ventilation may be necessary. This machine helps the baby breathe.
-
Surfactant Therapy: Administering surfactant can improve lung function. It helps keep the airways open.
-
Nutritional Support: Proper nutrition is crucial for growth and development. Special feeding techniques may be used.
-
Monitoring and Follow-up: Regular check-ups are essential. Doctors monitor lung function and overall health.
Prognosis and Long-term Outcomes
The long-term outlook for infants with WMS varies. Here are some factors that influence prognosis:
-
Severity of Symptoms: The severity of initial symptoms can impact long-term outcomes. Mild cases have a better prognosis.
-
Response to Treatment: How well an infant responds to treatment plays a crucial role. Effective management can improve outcomes.
-
Chronic Lung Disease: Some infants may develop chronic lung disease. This requires ongoing medical care.
-
Developmental Delays: There may be developmental delays. Early intervention programs can help.
-
Growth and Nutrition: Proper growth and nutrition are vital. Infants need adequate calories and nutrients.
Research and Future Directions
Ongoing research aims to improve understanding and treatment of WMS. Here are some areas of focus:
-
Genetic Studies: Researchers are exploring genetic factors. Identifying genes involved could lead to targeted therapies.
-
Improved Diagnostic Tools: New diagnostic methods are being developed. These aim to detect WMS earlier and more accurately.
-
Better Treatments: Scientists are working on new treatments. These could improve lung function and overall outcomes.
-
Preventive Measures: Research is focused on prevention. This includes strategies to reduce premature births.
-
Long-term Studies: Long-term studies are tracking outcomes. This helps understand the impact of WMS over time.
Understanding Wilson-Mikity Syndrome
Wilson-Mikity Syndrome, a rare lung condition in newborns, often leaves parents and caregivers with many questions. Knowing the symptoms like rapid breathing, cyanosis, and poor feeding can help in early detection. While the exact cause remains unknown, premature birth is a significant risk factor. Treatment usually involves oxygen therapy and sometimes mechanical ventilation.
Early intervention and regular monitoring are crucial for managing this condition. Advances in neonatal care have improved outcomes, but ongoing research is essential for better understanding and treatment. Support from healthcare professionals and connecting with other families facing similar challenges can provide much-needed comfort.
Staying informed and proactive can make a big difference in the lives of those affected by Wilson-Mikity Syndrome. Always consult healthcare providers for the most accurate and personalized advice.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.